- Joined
- Mar 20, 2013
- Messages
- 1,920
- Reaction score
- 3,532
I have a case of a pT1(4cm)N0MO Grade 2 sarcoma s/p resection by a good surg onc. Margins 4mm in two areas (deep and anterior), 1 mm "superficial" margin that surg onc feels is artifactually close (he took some skin). This was a superficial sarcoma in an obese leg. Just barely touched deep fascia but did not invade into muscle though surg onc took some muscle. Tumor involved saphenous vein and it had to be ligated.
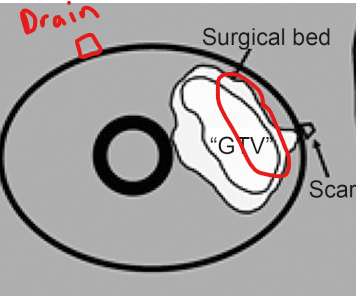
Patient already has some minor distal edema.
I took a cartoon of a sarcoma from a paper and edited. My patients disease/operative bed goes no where close to deep bone so operative bed is in red. in my patient the red surgical bed is superficial. However, the drain is almost medial/midline. A nice little tangent plan will cover the operative bed well, but I'm concerned that if I treat the drain site it will increase lymphedema risk more. Do I have to cover this drain site? Is is worth it to maybe put an electron patch there? Or just forgo it the drain site.
Any thoughts are appreciated.
Patient already has some minor distal edema.
I took a cartoon of a sarcoma from a paper and edited. My patients disease/operative bed goes no where close to deep bone so operative bed is in red. in my patient the red surgical bed is superficial. However, the drain is almost medial/midline. A nice little tangent plan will cover the operative bed well, but I'm concerned that if I treat the drain site it will increase lymphedema risk more. Do I have to cover this drain site? Is is worth it to maybe put an electron patch there? Or just forgo it the drain site.
Any thoughts are appreciated.

