- Joined
- Apr 18, 2011
- Messages
- 135
- Reaction score
- 33
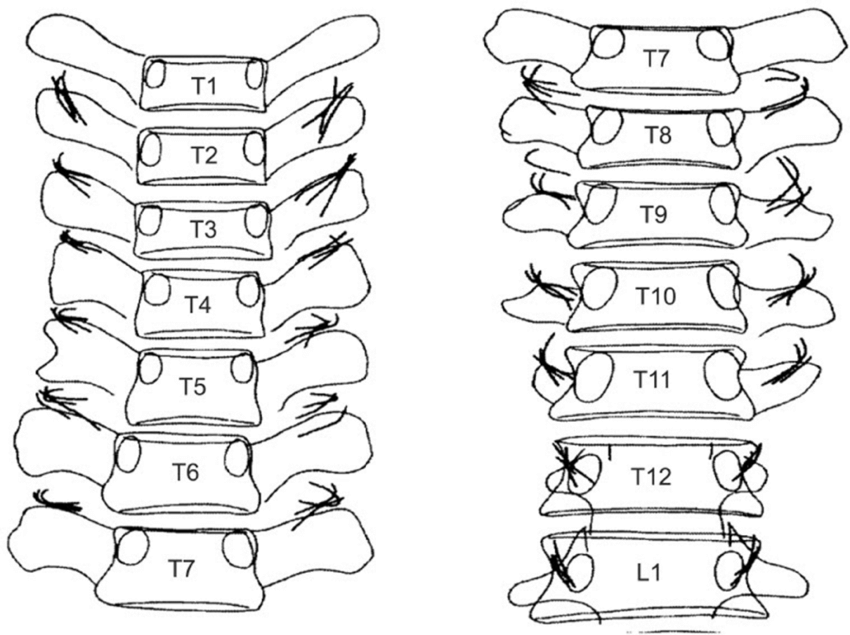
Hi all- I don’t have too much experience with treating thoracic facetogenic pain, and I’ve heard varying techniques. Thoughts appreciated.
Side note- WTF are the transverse processes so hard to see?!
Side note- WTF are the transverse processes so hard to see?!
