Dose matters...Just say "no" to weak sauce, ghetto juice PRP...
Acta Orthop Traumatol Turc. 2023 Jul;57(4):148-153.
doi: 10.5152/j.aott.2023.22077.
Factors affecting the features of platelet-rich plasma in patients with knee osteoarthritis
Sezen Karaborklu Argut 1,
Derya Celik 2,
Omer Naci Naci Ergin 2,
Onder Ismet Kilicoglu 3
Affiliations expand
Abstract
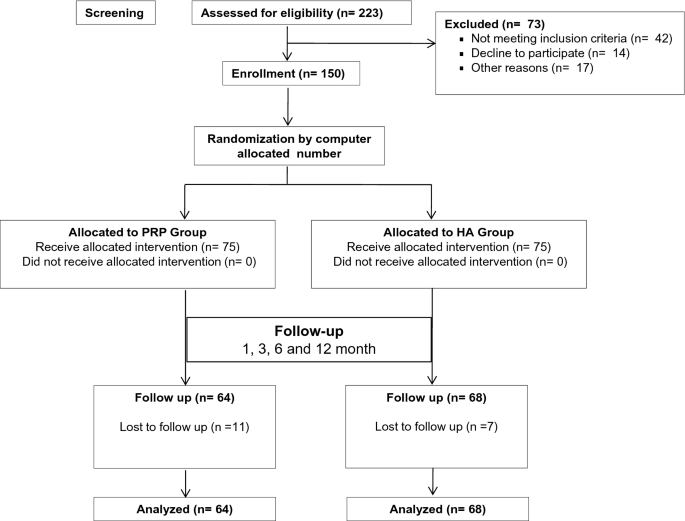
Objective: The aim of this study was to present an analysis of platelet-rich plasma obtained from patients with knee osteoarthritis and reveal the factors affecting its features.
Methods: A total of 62 patients (mean age: 56.68 ± 7.13 years) with symptomatic knee osteoarthritis were included in this study. Age (years), gender, height (m), weight (kg), body mass index (kg/m2), duration of symptoms, smoking status, smoking index, general health status, and physical activity scores were recorded. Whole blood and platelet-rich plasma cell counts were performed with a hematology analyzer. White blood cell, red blood cell, and platelet counts were recorded. According to the dose of injected platelets, efficiency of the procedure, purity of platelet-rich plasma, and activation classification, dose of platelets, efficiency of the procedure (platelet recovery rate, %), and purity of the obtained platelet-rich plasma product (relative composition in platelets, %) were calculated. Correlation analysis between the features of platelet-rich plasma and the patient-related variables, including age, gender, body mass index, smoking status, smoking index, presence of other health conditions, physical activity scores, duration of symptoms, and pain levels, was performed.
Results: Dose of injected platelets, efficiency of the procedure, purity of platelet-rich plasma, and activation analysis showed that the dose of injected platelets was 3.25 billion, the efficiency of the process was 77%, and the purity rate of the platelet-rich plasma was 98.4%. Platelet-rich plasma platelet count was correlated with whole blood platelet count (r = 0.81, P < .001), whole blood white blood cell count (r = 0.39, P = .002), smoking status (r = 0.56, P = .03), smoking index (r = -0.63, P = .002), and the presence of hypertension (r = -0.31, P=.04). Platelet-rich plasma white blood cell and purity of platelet-rich plasma were correlated with the smoking status of the patients (r = 0.52, P = .01; r = 0.64, P = .003, respectively).
Conclusion: This study has demonstrated that high dose and very pure platelet-rich plasma with medium efficiency was yielded with this platelet-rich plasma preparation procedure; whole blood platelet count, the presence of hypertension, and the smoking status of patients affect the features of the obtained platelet-rich plasma.
Level of evidence: Level IV, Diagnostic Study.
Key takeaways:
- Platelet count in whole blood (Wb_Plt) strongly correlates with platelet count in PRP (PRP_Plt). This is expected, as PRP is prepared by centrifuging whole blood to enrich the platelet fraction.
- White blood cell count in whole blood (Wb_WBC) and red blood cell count in whole blood (Wb_RBC)** are also correlated with PRP_Plt, but to a lesser extent. This suggests that other factors, such as the centrifugation protocol, may also play a role in determining PRP_Plt.
- Platelet distribution width (Wb_Pdw) is negatively correlated with PRP_Plt. This means that patients with narrower platelet distributions tend to have higher PRP_Plt.
- Gender, age, and BMI correlate with PRP_Plt, but the correlations are weaker.
- Dose of injected platelets, process efficiency, and PRP purity are all positively correlated. This suggests that these factors are all important for achieving high-quality PRP.
The heatmap shows that several patient-related variables correlate with PRP quality. This suggests that it is crucial to consider these variables when preparing PRP for clinical use.
Here are some specific recommendations for how the heatmap can be used to improve PRP quality:
- Select patients with high platelet counts and narrow platelet distributions.
- Use a centrifugation protocol that is optimized for platelet enrichment.
- Monitor the efficiency of the PRP preparation process and make adjustments as needed.
- Use a quality control protocol to ensure that the PRP is pure and meets all required standards.