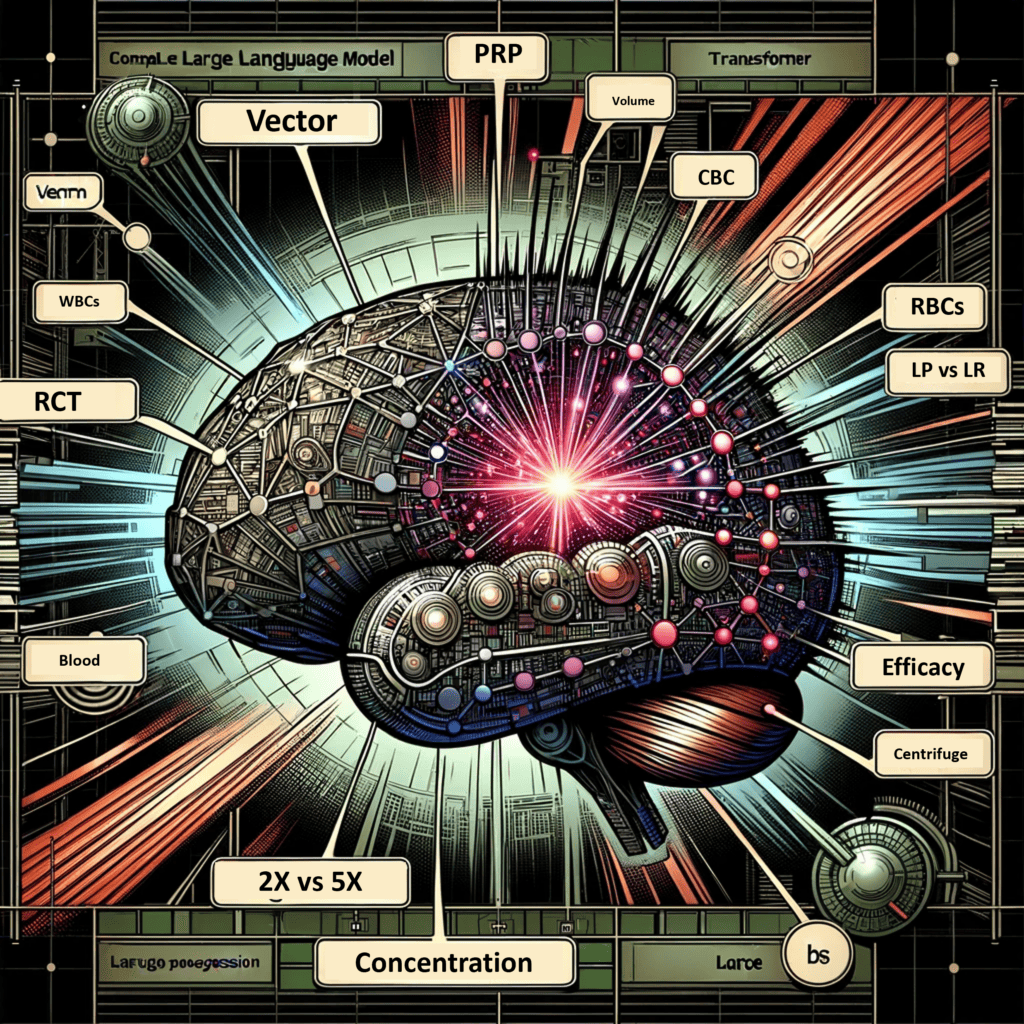
If you believe that PRP's treatment effects are placebo, do you also believe that potential complications are nocebo? Why or why not? Can a placebo be "not biologically active" but simultaneously cause objective tissue changes?
If you told me that my regen complications were all in my head, I'd be pissed...
The present, more comprehensive study confirms the previous preliminary analysis that treating CMIs with PRP may be associated with HO.

pubmed.ncbi.nlm.nih.gov
Am J Sports Med
2024 Jan;52(1):54-59.
doi: 10.1177/03635465231209509.
Heterotopic Ossification and Platelet-Rich Plasma in Core Muscle Injuries: A Single-Institution Experience Over 6 Years
Alexander E Poor 1 2 3,
Adam C Zoga 2,
Alec Warren 1,
Leigh C Waters 1,
Louis Vilotti 1,
Garrison P Bentz 1,
William C Meyers 1 2 3 4
Affiliations expand
Abstract
Background: A 2015 study of platelet-rich plasma (PRP) for groin injuries in National Football League (NFL) players alerted the authors to the possibility that PRP is associated with heterotopic ossification (HO). The current study of athletes seen between 2014 and 2019 provides a more comprehensive analysis of that observation.
Purpose/hypothesis: This report describes the early results of groin surgery for athletes who had experienced failed PRP therapy performed by different practitioners and with an assortment of PRP techniques. The primary goal of this cohort study was to determine short-term clinical outcomes after surgery of PRP-treated patients. It was hypothesized that previous PRP treatment would be associated with the presence of HO among patients with core muscle injuries (CMIs).
Study design: Cohort study; Level of evidence, 3.
Methods: All athletes seen at 1 institution and identified at their first visit as having received PRP for a CMI were followed and compared with patients with a CMI who had not previously received PRP. Although in many cases HO was observed on clinical examination or imaging, HO was identified intraoperatively in all surgical cases and confirmed pathologically. Successful surgery was defined as return to play at previously high levels of performance or greater as determined by the athletes' own assessments. All patients who had received PRP were followed for ≥2 years.
Results: Among 3642 patients with a new CMI seen between 2014 and 2019, 68 (1.9%) patients developed HO within the core muscles and/or adjacent soft tissues. Of the 68 patients, 60 (88.2%) were men, and the mean age was 34.5 years. Of the 68 patients, 62 (91.2%) were athletes and 44 (64.7%) had been treated previously with PRP. HO was observed in 24 (0.7%) patients without previous PRP treatment. Three athletes who received PRP retired early from sports because of HO and scar issues. In total, 22 of 28 (78.6%) NFL players who received PRP developed HO, compared with 0 (0%) of 28 randomly selected, age-, position-, and injury-matched NFL players. After surgical repair, 3-month success rates were 67.9% and 96.4%, respectively, in the PRP and non-PRP groups (
P = .006). By 6 months postoperatively, PRP-treated patients were back to similarly high success rates compared with the non-PRP cohort. Scar tissue issues played a prominent role in the relative delay in definitive success.
Conclusion: The present, more comprehensive study confirms the previous preliminary analysis that treating CMIs with PRP may be associated with HO.
Keywords: core muscle injuries; heterotopic ossification; platelet-rich plasma.
This study investigates the relationship between platelet-rich plasma (PRP) treatment and the development of heterotopic ossification (HO) in patients with core muscle injuries (CMIs). HO involves abnormal bone growth within muscles and other tissues. The study, conducted over 6 years at a single institution, focused on athletes, many from the NFL, who had failed PRP therapy for groin injuries and then underwent surgery.
Key findings include:
- Out of 3642 patients with CMIs, 68 (1.9%) developed HO. Among these, 44 (64.7%) had received PRP treatment.
- The study observed a higher incidence of HO in patients treated with PRP than those without PRP (40.7% vs. 0.7%).
- Post-surgery, PRP-treated patients initially had lower success rates at three months than non-PRP patients, but success rates evened out by six months.
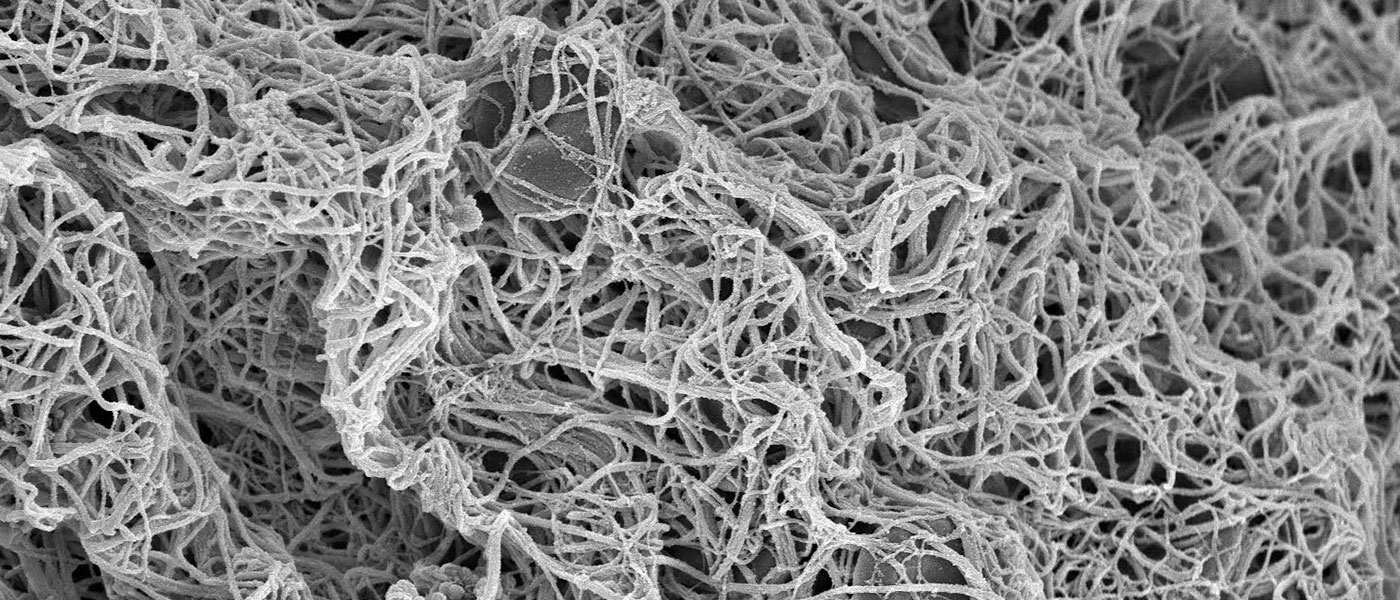
- PRP treatment was associated with delayed rehabilitation due to issues like scarring and thickening of muscle tissue.
- The study suggests a potential link between PRP treatment and the development of HO in patients with CMIs, particularly among athletes. However, it also notes the limitations of its findings due to the non-randomized, retrospective nature of the study and the potential bias from focusing on patients who had unsuccessful PRP treatments. The researchers caution against concluding that PRP directly causes HO, but the association they observed suggests the need for further investigation and careful consideration before using PRP for CMIs.