Just cause one pays the franchise fee doesn't mean their McPRP is any better than homemade PRP.
Cell counts and hoods don't matter except for marketing.
Don't be anti-scientific and mislead junior practitioners like
@lobelsteve into an inflated sense of confidence about his ignorance. He will hurt people. No one can just bombastically say, "Hey, my ghetto juice, weak sauce PRP is just has good as your higher concentration, dose characterized ortho-biologic."
In God we trust; everyone else please bring a pre-/post- CBC before making wild ass claims. Just like anything else in medicine, you need to choose the right tissue product, at the right time, for the right patient.
1) Cell counts matter because dose matters.
2) Sterility and preparation matter because if you're injecting IO, intradiscal, or epidural you can have complications from contamination.
Int Orthop. 2022 Oct;46(10):2219-2228.
doi: 10.1007/s00264-022-05524-9. Epub 2022 Aug 6.
Percutaneous autologous bone marrow concentrate for knee osteoarthritis: patient-reported outcomes and progenitor cell content
Christopher J Centeno 1 2,
Dustin R Berger 2,
Brandon T Money 1,
Ehren Dodson 2,
Christopher W Urbanek 1,
Neven J Steinmetz 3
Affiliations expand
Free PMC article
Abstract
Purpose: Knee osteoarthritis (OA) is a common, progressively debilitating joint disease, and the intra-articular injection of autologous bone marrow concentrate (BMC) may offer a minimally invasive method of harnessing the body's own connective tissue progenitor cells to counteract accompanying degenerative effects of the disease. However, the extent to which the progenitor cell content of BMC influences treatment outcomes is unclear. We sought to determine whether patient-reported outcome measures associated with BMC treatment for knee OA are related to the concentration of progenitor cells provided.
Methods: In the present study, 65 patients (72 knees) underwent treatment for knee OA with autologous BMC and self-reported their outcomes for up to one year using follow-up questionnaires tracking function, pain, and percent improvement. A small fraction of each patient's BMC sample was reserved for quantification with a haematological analyzer and cryopreserved for subsequent analysis of potential connective tissue progenitor cells using a colony-forming unit fibroblast (CFU-F) assay.
Results: Patients reported significant increases in function and overall percent improvement in addition to decreases in pain relative to baseline levels following treatment with autologous BMC that persisted through 12 months. Patients reporting improved outcomes (46 of 72 knees) received BMC injections having higher CFU-F concentrations than non-responding patients (21.1×103 ± 12.4×103 vs 14.3×103 ± 7.0 x103 CFU-F per mL). A progenitor cell concentration of 18×103 CFU-F per mL of BMC was found to best differentiate responders from non-responders.
Conclusion: This study provides supportive evidence for using autologous BMC in the minimally invasive treatment of knee OA and suggests that increased progenitor cell content leads to improved treatment outcomes.
Trial registration: ClinicalTrials.gov Identifier:
NCT03011398, 1/7/17.
Keywords: Bone marrow concentrate (BMC); Colony-forming unit fibroblast (CFU-F); Connective tissue progenitor cells; Knee osteoarthritis (OA).
© 2022. The Author(s).
Cartilage. 2023 Jun 22;19476035231166127.
doi: 10.1177/19476035231166127. Online ahead of print.
Knee Osteoarthritis: Clinical and MRI Outcomes After Multiple Intra-Articular Injections With Expanded Autologous Adipose-Derived Stromal Cells or Platelet-Rich Plasma
Miguel A Khoury 1,
Karim Chamari 1,
Montassar Tabben 1,
Khalid Alkhelaifi 1,
Emmanuel Papacostas 1,
Theodorakys Marín Fermín 1,
Markus Laupheimer 1,
Pieter D Hooghe 1
Affiliations expand
Abstract
Objective: To directly compare clinical and MRI outcomes of multiple intra-articular injections of adipose-derived stromal cells (ASCs) or platelet-rich plasma (PRP) in patients with knee osteoarthritis (OA).
Design: We retrospectively compared 24-month outcomes in (1) 27 patients receiving 3-monthly intra-articular injections with a total of 43.8 million ASCs and (2) 23 patients receiving 3-monthly injections of 3-ml preparation of PRP. All patients had Kellgren-Lawrence grade 1, 2, or 3 knee OA with failed conservative medical therapy. The Numeric Pain Rating Scale (NPRS) scores; Knee injury and Osteoarthritis Outcome Score (KOOS) at baseline, 6, 12, and 24 months after the first injection; and the MRI Osteoarthritis Knee Score (MOAKS) at 12 and 24 months were considered as outcomes.
Results: No major complications occurred in any patient. Both groups significantly improved in pain NPRS score and KOOS at 6 months. At 12- and 24-month evaluations, the ASC group significantly decreased scores to a greater degree (
P < 0.001) than the PRP group. MOAKS scores indicated a decrease in disease progression in the ASC group.
Conclusion: Both ASCs and PRP were safe and resulted in clinical improvement in patients with knee OA at 6 months; however, at 12 and 24 months, ASCs outperformed leukocyte-poor PRP in clinical and radiological outcomes.
Keywords: adipose-derived stromal cells; cartilage injury; intra-articular injection; osteoarthritic knee pain; stem cells.
Acta Biomed. 2022 Oct 26;93(5):e2022222.
doi: 10.23750/abm.v93i5.12845.
Clinical and functional evaluation of bone marrow aspirate concentrate vs autologous conditioned serum in the treatment of knee osteoarthritis
Matteo Vitali 1,
Marco Ometti 2,
Pierluigi Pironti 3,
Damiano Salvato 4,
Alice Sandrucci 5,
Orlando Leone 6,
Vincenzo Salini 7
Affiliations expand
Free PMC article
Abstract
Background and aim: The aim of this study was to compare the efficacy of a single Bone Marrow Aspirate Concentrate (BMAC) with a cycle of 4 Autologous Conditioned Serum (ACS) injections in the treatment of early-stage knee osteoarthritis (OA).
Methods: Two groups of 12 patients with degenerative knee OA were treated with a single BMAC injection and with a cycle of 4 ACS injections respectively. Follow-up was set at baseline (t0), one-month (t1) and six-months (t2) evaluating VAS for pain, WOMAC index and range of motion (ROM).
Results: We reported a significant improvement in WOMAC after BMAC injection both at t1 (p= 0,001) as well as t2 (p< 0,001), plus a reduction of VAS values in BMAC group at six months follow-up (p = 0,024). In contrast, no significant differences in ROM between the two groups were observed.
Conclusions: Both the approaches are safe and effective in the treatment of knee OA, with a major efficacy of BMAC.
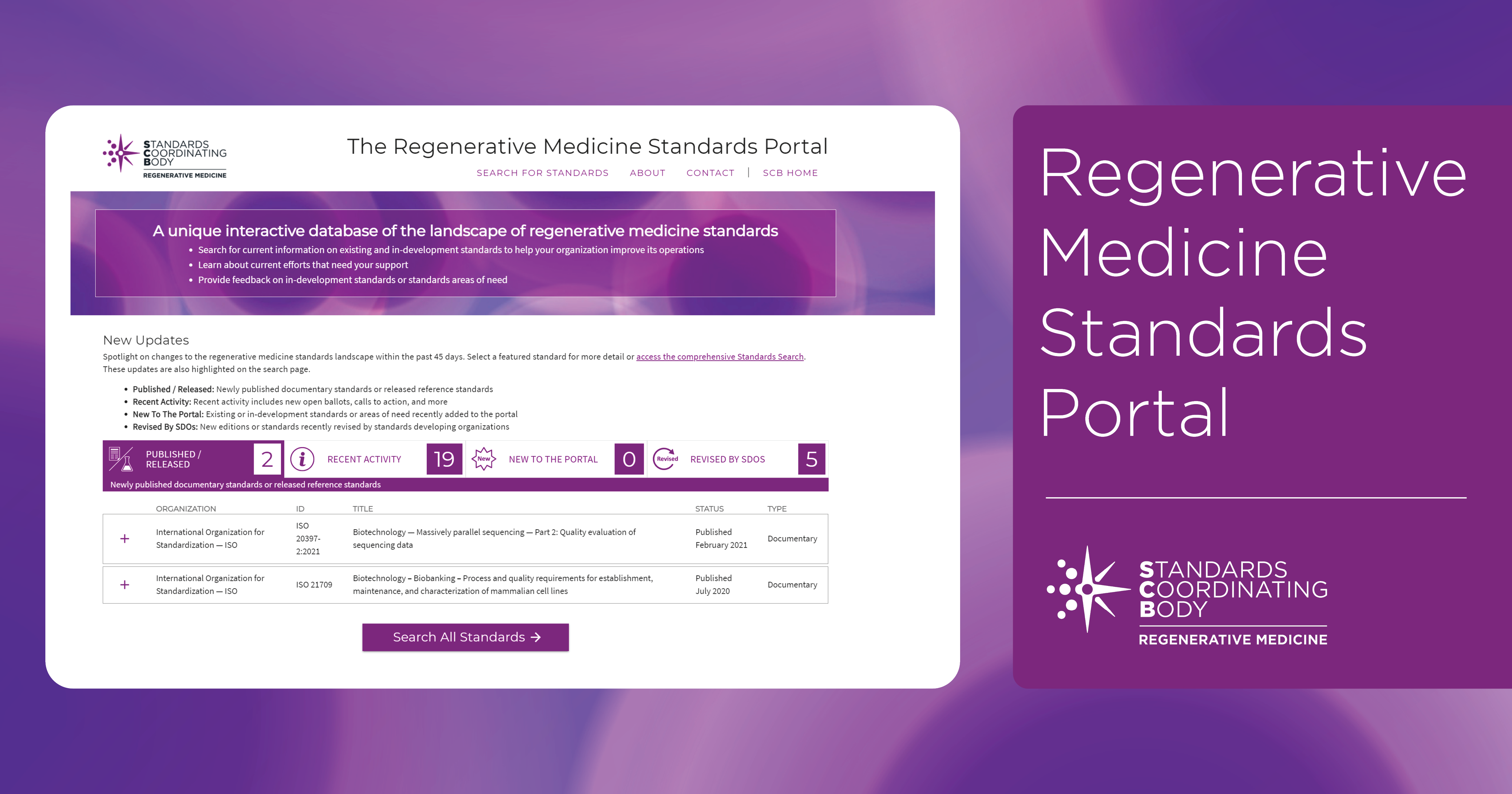
portal.standardscoordinatingbody.org
www.ncbi.nlm.nih.gov

interventionalorthobiologics.org








