Curious as to what was the impetus for radiation oncology to separate from the house of radiology? What were the key factors involved in the separation? Who were the key thought leaders in radiation oncology that led to the separation? Do you think that radiation oncology could have still been as successful if it were a subspecialty of radiology?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Split of radiation oncology from diagnostic radiology
- Thread starter irwarrior
- Start date
I don’t know about the time of the split but currently we would be way better off with radiology in charge and radonc as a fellowship
I'm not so sure. having people be in charge who know nothing about what we do is tricky. have seen this in places where radiology is still in charge of rad onc. was a disaster. big picture/national level may be different than individual departments, but does not give me any reason to have faith.
- Joined
- Apr 21, 2011
- Messages
- 3,622
- Reaction score
- 9,248
I think we’d be much better off, if only because when it’s slow (most of the time, for most rad oncs), you could be reading diagnostic scans to make some side cash.
And with how technical the field has become, reading scans is really the most important thing we have to do/is VERY poorly taught in most residencies.
And with how technical the field has become, reading scans is really the most important thing we have to do/is VERY poorly taught in most residencies.
MidwestRadOnc
Full Member
- Joined
- Dec 20, 2023
- Messages
- 389
- Reaction score
- 977
have seen this in places where radiology is still in charge of rad onc. was a disaster.
Wait until you've seen med onc in charge.
How much of your residency is taught in scan interpretation? Do you have dedicated months of training?I think we’d be much better off, if only because when it’s slow (most of the time, for most rad oncs), you could be reading diagnostic scans to make some side cash.
And with how technical the field has become, reading scans is really the most important thing we have to do/is VERY poorly taught in most residencies.
- Joined
- Dec 17, 2007
- Messages
- 3,390
- Reaction score
- 4,403
Well, the counterargument is that once medonc discovers that they can make money for themselves by sending patients to radonc for treatment, it can be beneficial for both sides...Wait until you've seen med onc in charge.
Oh this is a different point. I meant more rad onc as is with radiology in charge.I think we’d be much better off, if only because when it’s slow (most of the time, for most rad oncs), you could be reading diagnostic scans to make some side cash.
And with how technical the field has become, reading scans is really the most important thing we have to do/is VERY poorly taught in most residencies.
- Joined
- Apr 21, 2011
- Messages
- 3,622
- Reaction score
- 9,248
Mine was none. Zero. Zip.How much of your residency is taught in scan interpretation? Do you have dedicated months of training?
All learn on the job.
- Joined
- Oct 4, 2017
- Messages
- 5,017
- Reaction score
- 9,784
in early 2000s radonc still mostly felied on bony landmarks to define portals.Impressive to gain all that knowledge of CT/MRI head to toe on your own. The anatomy can be quite challenging even with dedicated DR training.
My residency had lectures by radiology faculty to go over normal anatomy, but most of the learning was done "on the job."
I feel as a radonc I have a good understanding of CT cancer anatomy, but please don't ask me too many non-cancer questions.
I feel as a radonc I have a good understanding of CT cancer anatomy, but please don't ask me too many non-cancer questions.
- Joined
- Sep 20, 2004
- Messages
- 11,742
- Reaction score
- 11,834
I know at least in the early 70s, plenty of boomers were getting dual boarded in both at graduationCurious as to what was the impetus for radiation oncology to separate from the house of radiology? What were the key factors involved in the separation? Who were the key thought leaders in radiation oncology that led to the separation? Do you think that radiation oncology could have still been as successful if it were a subspecialty of radiology?
MidwestRadOnc
Full Member
- Joined
- Dec 20, 2023
- Messages
- 389
- Reaction score
- 977
Well, the counterargument is that once medonc discovers that they can make money for themselves by sending patients to radonc for treatment, it can be beneficial for both sides...
What's more likely in a med onc (or urology)- owned business?
(1) The medoncs refer a ton of patients to rad onc and let them keep all of the pro and a little bit of the tech to incentivize them because they are so nice.
or
(2) They employee a rad onc at the lowest salary or RVU rate they can get on the open market and have them produce as much as possible or they are fired.
If you find yourself in situation (1), I would be very worried about it quickly becoming situation (2).
MidwestRadOnc
Full Member
- Joined
- Dec 20, 2023
- Messages
- 389
- Reaction score
- 977
Impressive to gain all that knowledge of CT/MRI head to toe on your own. The anatomy can be quite challenging even with dedicated DR training.
I have seen this frequently among my peers. An overconfidence of image interpretation ability despite no formal training. How many of us can even properly read a chest xray if we are honest? I can't.
Yes, it feels satisfying sometimes to call radiology because you've discovered an additional 3mm brain met and they have to amend the report, but no delusions of being anywhere near a DR here.
- Joined
- Apr 28, 2005
- Messages
- 1,198
- Reaction score
- 3,441
I have seen this frequently among my peers. An overconfidence of image interpretation ability despite no formal training. How many of us can even properly read a chest xray if we are honest? I can't.
Yes, it feels satisfying sometimes to call radiology because you've discovered an additional 3mm brain met and they have to amend the report, but no delusions of being anywhere near a DR here.
I’ve often thought rad onc could benefit from some formal training in CTs and especially MRIs.
- Joined
- Jul 7, 2008
- Messages
- 1,348
- Reaction score
- 876
This is how some degree of subspecialization (organ-site) can help whether academic or private. Attending high volume disease site tumor boards every week for years should improve image interpretation/finer anatomy points.I’ve often thought rad onc could benefit from some formal training in CTs and especially MRIs.
Starting out I would occasionally curbside rads-- it's a really rare case (eg: new nuc med test that wasn't read well) I feel the need to do that anymore within my primary organ sites.
MidwestRadOnc
Full Member
- Joined
- Dec 20, 2023
- Messages
- 389
- Reaction score
- 977
If you treat prostate with modern techniques, you should probably know how to read a mpMRI as good as a DR (or reading MRI for image-guided cervix HDR). How many rad oncs can honestly say that? That's an example of where some formal DR training would be helpful. I've taught myself a fair amount, but I'd like to get some real CME on things like this.
- Joined
- Oct 4, 2017
- Messages
- 5,017
- Reaction score
- 9,784
Agree, but for antrying non malignant, I am worthlessThis is how some degree of subspecialization (organ-site) can help whether academic or private. Attending high volume disease site tumor boards every week for years should improve image interpretation/finer anatomy points.
Starting out I would occasionally curbside rads-- it's a really rare case (eg: new nuc med test that wasn't read well) I feel the need to do that anymore within my primary organ sites.
- Joined
- Jul 7, 2008
- Messages
- 1,348
- Reaction score
- 876
Oh I don’t want to deal with diagnostic reads at all. Id rather focus on expanding RT indications/reimbursement/physician control and appropriate training #sAgree, but for antrying non malignant, I am worthless
Oh I don’t want to deal with diagnostic reads at all. Id rather focus on expanding RT indications/reimbursement/physician control and appropriate training #s
agree. This would be a totally different field if we did diagnostic rads. Not what I signed up for or am interested in.
- Joined
- Nov 2, 2019
- Messages
- 3,497
- Reaction score
- 14,498
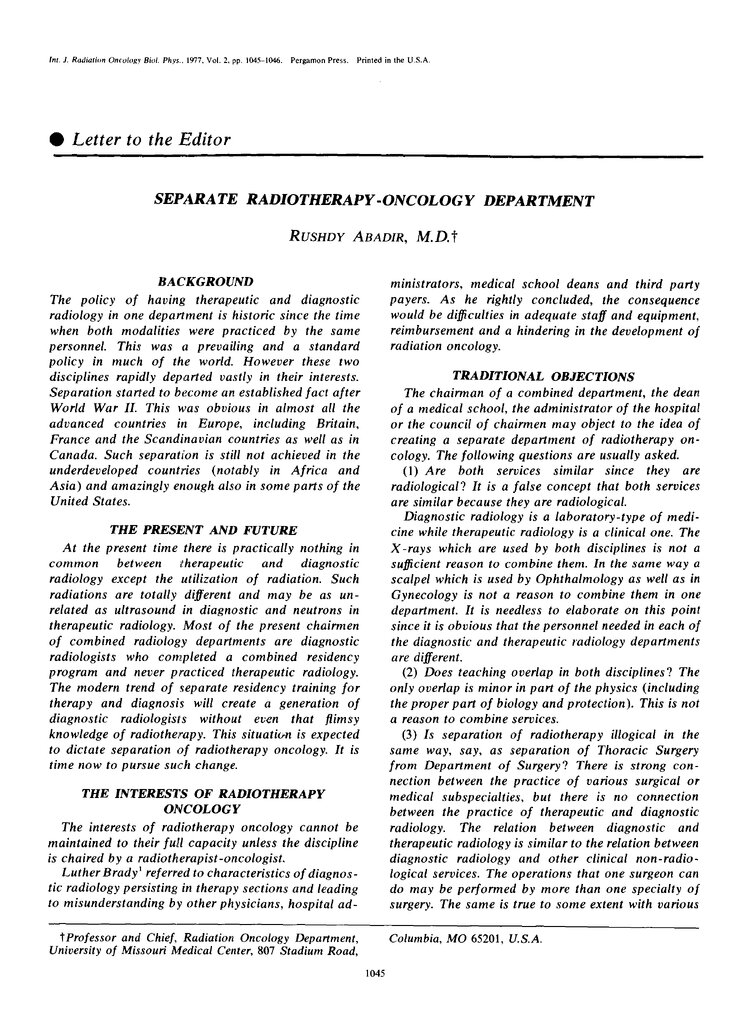
Relevant paper from the Red Journal archives, 1977:

- Joined
- Sep 20, 2004
- Messages
- 11,742
- Reaction score
- 11,834
This x100000. We are our own worst enemy.Oh I don’t want to deal with diagnostic reads at all. Id rather focus on expanding RT indications/reimbursement/physician control and appropriate training #s
Secular growth has kept rads in the game and then some, we have been focused on trying to reduce/eliminate our footprint while simultaneously pumping out more grads
- Joined
- Oct 24, 2010
- Messages
- 3,509
- Reaction score
- 6,356
I see you dusted off the journal from the shelf! 😂… were they still using rads back then?
Last edited:
To add some clarification
-we would be better off under radiology for 3 reasons
—they understand supply and demand. They have had minimal expansion. This would cap our own numbers.
—obvious fall back plan to do DR if radonc saturated.
—we would be better at radonc with formal rad training
Downside is that you can be marginalized with others in control . Certainly the 5 radoncs in a 50 doc combined department will not have equal footing. But how much control does average radonc have now ?
-we would be better off under radiology for 3 reasons
—they understand supply and demand. They have had minimal expansion. This would cap our own numbers.
—obvious fall back plan to do DR if radonc saturated.
—we would be better at radonc with formal rad training
Downside is that you can be marginalized with others in control . Certainly the 5 radoncs in a 50 doc combined department will not have equal footing. But how much control does average radonc have now ?
- Joined
- Apr 21, 2011
- Messages
- 3,622
- Reaction score
- 9,248
Our "standard" (there is considerable heterogeneity betwixt residencies) curriculum is completely ridiculous.To add some clarification
-we would be better off under radiology for 3 reasons
—they understand supply and demand. They have had minimal expansion. This would cap our own numbers.
—obvious fall back plan to do DR if radonc saturated.
—we would be better at radonc with formal rad training
Downside is that you can be marginalized with others in control . Certainly the 5 radoncs in a 50 doc combined department will not have equal footing. But how much control does average radonc have now ?
Make sure you know what an auger electron is and be sure to memorize fallopian tube staging, but will anyone ever teach/ask you to identify a common bile duct on a scan? Completely lost the script.
- Joined
- Apr 28, 2005
- Messages
- 1,198
- Reaction score
- 3,441
It not unreasonable to say that rad onc (from the perspective of the practicing physicians who actually do the work not the conglomerate hospital systems and departments) would be in a much better position if it were a fellowship after general rads. Rad onc in the last 10 to 15 years has demonstrated that it can not govern itself well as stand alone specialty for the majority of those who practice.
- Joined
- Apr 28, 2005
- Messages
- 1,198
- Reaction score
- 3,441
" —we would be better at radonc with formal rad training "
From:
MidwestRadOnc
Full Member
- Joined
- Dec 20, 2023
- Messages
- 389
- Reaction score
- 977
- Joined
- Nov 2, 2019
- Messages
- 3,497
- Reaction score
- 14,498
Anyone want to take a guess at how many of these volumes come from people considered esteemed "Key Opinion Leaders"?
This looks like an argument against the "academic main campus single disease site expert" to me...
- Joined
- Apr 21, 2011
- Messages
- 3,622
- Reaction score
- 9,248
But what if there was subclinical erosion through the skull, skin, and in to the atmosphere?(E) is peak boomer.
Do you know that there wasn't?
- Joined
- Feb 17, 2017
- Messages
- 468
- Reaction score
- 732
Clearly the error is that they forgot to place the bolus!But what if there was subclinical erosion through the skull, skin, and in to the atmosphere?
Do you know that there wasn't?
- Joined
- Oct 10, 2011
- Messages
- 8,624
- Reaction score
- 10,698
Good news! Volumes don't matter in GBM. As big or as small as you want, outcomes are all the same!
- Joined
- Jul 16, 2019
- Messages
- 218
- Reaction score
- 453
You are correct, we all could do better at image interpretation.Oh I don’t want to deal with diagnostic reads at all. Id rather focus on expanding RT indications/reimbursement/physician control and appropriate training #s
Personally though, I think it can be done without doing a full residency in both. I am sure there are good reasons that radiation oncology is no longer a subset of diagnostic radiology. I have been to the RSNA meeting before, and I was really impressed. They make the ASTRO meeting look like a traveling carnival compared to Disneyland. The ASCO meeting is similarly impressive in scale, but totally boring in the exhibit hall - no machines on display!
Not that it couldn't be done, but it is nearly impossible to keep adequately up to date in 2 or 3 specialties, especially if you try to be a generalist in each. At the end of the day, people will be drawn more toward one and end up developing that skillset more, which I think is why the fields split. The breadth and depth of both have increased a lot since. There are imaging fellowships now for just breast, for instance.
I know a guy who did 2 years diagnostic and 1 year therapy in his radiology residency. That was it - 2 fields in 3 years. He was a very good rad onc by the way. That was in the 70s though, when MRI, PETCT, and CT simulation were not widely available, if at all. There was no SBRT, IMRT, 3D, CBCT, HDR, or most of the other things that we now take for granted. Cobalt-60 was commonplace. Both fields have gotten a lot more sophisticated and nuanced since the 1970s - it's been 50 years now.
Politically, if the fields were merged, we can all guess who would get listened to more and who steers the ship. If ASTRO doesn't represent your interests now, how well would the RSNA do?
- Joined
- Oct 4, 2017
- Messages
- 5,017
- Reaction score
- 9,784
We don’t need Astro to represent our interests so much as stop actively working against them.You are correct, we all could do better at image interpretation.
Personally though, I think it can be done without doing a full residency in both. I am sure there are good reasons that radiation oncology is no longer a subset of diagnostic radiology. I have been to the RSNA meeting before, and I was really impressed. They make the ASTRO meeting look like a traveling carnival compared to Disneyland. The ASCO meeting is similarly impressive in scale, but totally boring in the exhibit hall - no machines on display!
Not that it couldn't be done, but it is nearly impossible to keep adequately up to date in 2 or 3 specialties, especially if you try to be a generalist in each. At the end of the day, people will be drawn more toward one and end up developing that skillset more, which I think is why the fields split. The breadth and depth of both have increased a lot since. There are imaging fellowships now for just breast, for instance.
I know a guy who did 2 years diagnostic and 1 year therapy in his radiology residency. That was it - 2 fields in 3 years. He was a very good rad onc by the way. That was in the 70s though, when MRI, PETCT, and CT simulation were not widely available, if at all. There was no SBRT, IMRT, 3D, CBCT, HDR, or most of the other things that we now take for granted. Cobalt-60 was commonplace. Both fields have gotten a lot more sophisticated and nuanced since the 1970s - it's been 50 years now.
Politically, if the fields were merged, we can all guess who would get listened to more and who steers the ship. If ASTRO doesn't represent your interests now, how well would the RSNA do?
Good read thank you for sharing this. it's interesting to think about how perceptions might now be different if we had maintained the designation 'therapeutic radiology' especially with respect to treating benign conditions.
- Joined
- Jun 21, 2022
- Messages
- 944
- Reaction score
- 3,286
MidwestRadOnc
Full Member
- Joined
- Dec 20, 2023
- Messages
- 389
- Reaction score
- 977
A good point.
The amount and quality of radiology training in med school is ridiculous given its paramount role in modern medicine.
I went to a highly regarded med school and graduated without knowing how to interpret a CXR or skeletal plain films at a basic level. I was not alone. I don't remember learning cross sectional anatomy on CT, instead still using Netter's ancient cartoons and anatomy lab. I don't think I ever saw a PET scan outside of my rad onc rotation. But large amounts of time were spent learning antiquated physical exam techniques.
And we spent probably a hundred hours at mandatory lectures and seminars involving public health and "social issues" in medicine. No education about the economics of medicine or running a practice, just that the government should manage and pay for it. But we definitely learned how not to be racist towards patients, and I'm thankful for that. I can't imagine how it is now. I mean, I came out about as anti-woke/DEI as possible and not totally convinced that vaccines are anything other than 100% perfect so clearly something was wrong in my education. Waiting to be re-educated soon...
- Joined
- Jun 21, 2022
- Messages
- 944
- Reaction score
- 3,286
But we definitely learned how not to be racist towards patients, and I'm thankful for that.
LOL did we though? Im not sure it took.
(I dont disagree with reprioritizing med ed topics in UGME).
You are correct, we all could do better at image interpretation.
Personally though, I think it can be done without doing a full residency in both. I am sure there are good reasons that radiation oncology is no longer a subset of diagnostic radiology. I have been to the RSNA meeting before, and I was really impressed. They make the ASTRO meeting look like a traveling carnival compared to Disneyland. The ASCO meeting is similarly impressive in scale, but totally boring in the exhibit hall - no machines on display!
We should be much more clear about goals of imaging education for radiation oncologists assuming weve moved past discussing a joint residency. I totally agree with you. Rad Oncs need to be really good at our narrow set of imaging interpretation indications, and these are very different than a general radiologist. One concern I have had recently is with 3D anatomy identification for on table adaptive treatments. I have seen more than one experienced attending mis-contour parts of the bowel anatomy, which can lead to serious toxicity in some cases. I would rather have ROs 100% competent at delineating a duodenum than being able to create a differential for duodenal disease based on an image.
Wallner is an interesting guy and I would enjoy reading his work but it makes me so angry. He spends all of his time criticizing training... after all, that is definitively not the ABRs responsibility. However, they do very little to test imaging competency. Images on oral boards are famous for being really poor quality. I rarely see these questions in OLA. I remember just a couple image questions if any on any of the many initial cert exams, in-service, etc.
Anyway, to his title... Id argue Im cool with IGRT. Maybe you should actually assess the status of our field on this skill instead of just hypothesizing it's not good and telling training programs to do better.
After all, the majority of the ABR's work is testing radiologists on image interpretation.
- Joined
- Dec 29, 2014
- Messages
- 338
- Reaction score
- 612
You'll have to define Academic for Rad Onc now. Not sure if it's the same on Radiology.Wonder what the ratio of academic/ private in rads vs radonc
I'm at a community satellite of large hospital system, hospital employed, with the rest of the main site academic. Am I in an academic job? Hell no. Am I in a private job? Sadly, hell no.
- Joined
- Nov 2, 2019
- Messages
- 3,497
- Reaction score
- 14,498
I'm entirely self-taught when it comes to reading diagnostic imaging. Obviously, I'm sure the majority of us can say that.A good point.
The amount and quality of radiology training in med school is ridiculous given its paramount role in modern medicine.
I went to a highly regarded med school and graduated without knowing how to interpret a CXR or skeletal plain films at a basic level. I was not alone. I don't remember learning cross sectional anatomy on CT, instead still using Netter's ancient cartoons and anatomy lab. I don't think I ever saw a PET scan outside of my rad onc rotation. But large amounts of time were spent learning antiquated physical exam techniques.
And we spent probably a hundred hours at mandatory lectures and seminars involving public health and "social issues" in medicine. No education about the economics of medicine or running a practice, just that the government should manage and pay for it. But we definitely learned how not to be racist towards patients, and I'm thankful for that. I can't imagine how it is now. I mean, I came out about as anti-woke/DEI as possible and not totally convinced that vaccines are anything other than 100% perfect so clearly something was wrong in my education. Waiting to be re-educated soon...
Fortunately, I trained deep into the "digital era". I'm a huge nerd, there are plentiful resources, and I cared very much about being "good" in a practical sense. I purchased/subscribed to various Radiology-training platforms that are relatively new (stuff like e-Anatomy). There's some amazing stuff out there.
I've had the unfortunate opportunity to work alongside, or take over a practice for, pre-Internet Boomer RadOncs. The ones that trained in the late 80s/early 90s.
The ones had had that "1980s Wall Street arrogance" energy that are also "self-taught", from the ground up, modern image reading and contouring.
I've seen things from them that will haunt me till I die. Just straight up missing giant tumors. Contouring the heart as a GTV. 1mm PTV expansions with no immobilization.
Then, in the rest of Medicine, many other types of physicians don't even try. Just straight up relying on the reports, because the focus of their specialty is elsewhere. It's not worth it to dedicate additional, personal time to having some "working ability" to read crazy new Radiology tech.
Unless an EMP takes out the grid and sends us back into the Stone Age, we're only going to rely on fancy new diagnostic imaging modalities more and more and more.
There needs to be a huge focus shift in med school and residency training to meet the need.
- Joined
- Apr 21, 2011
- Messages
- 3,622
- Reaction score
- 9,248
What if medical school was actually practical?
How many humans have you dissected since? How many citric acid cycles have you thought about? Phenylalanine, you hip to that?
Here's the **** that hurts, sickens, and kills people. Here are the causes, means of preventing, evaluation and management strategies for those things.
How many humans have you dissected since? How many citric acid cycles have you thought about? Phenylalanine, you hip to that?
Here's the **** that hurts, sickens, and kills people. Here are the causes, means of preventing, evaluation and management strategies for those things.
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
They could be all from the same "expert".Anyone want to take a guess at how many of these volumes come from people considered esteemed "Key Opinion Leaders"?
This looks like an argument against the "academic main campus single disease site expert" to me...
They could be all mine on the same patient.
I don't doubt they could be all yours.
Variability in contouring is massive and has no "Ground Truth".
Experts contour just as poorly as generalists...
MidwestRadOnc
Full Member
- Joined
- Dec 20, 2023
- Messages
- 389
- Reaction score
- 977
Experts contour just as poorly as generalists...
In many cases worse than. If you’ve ever seen a 20+ year site specific doc have to cover a different site, watch out.
Similar threads
- Replies
- 45
- Views
- 3K
