- Joined
- Jun 20, 2013
- Messages
- 320
- Reaction score
- 221
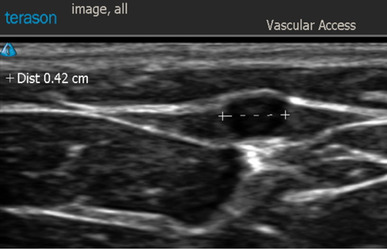
I believe @pgg and @PpfSuxTube mentioned this in another thread and I wanted to have one to discuss this topic. How many people do this? What doses do you use? I know our vascular people do 200mcg of nitro and 1mg of verapamil into their sheaths to dilate. For people who inject nitro peri-arterial with the local do you get any hypotension? Not sure how much or if any would be absorbed or go systemically. I'm thinking for the sick tiny artery people this may be of some benefit. Anyone use verapamil?