Neoadjuvant durvalumab plus radiation versus durvalumab alone in stages I–III non-small cell lung cancer: survival outcomes and molecular correlates of a randomized phase II trial - Nature Communications
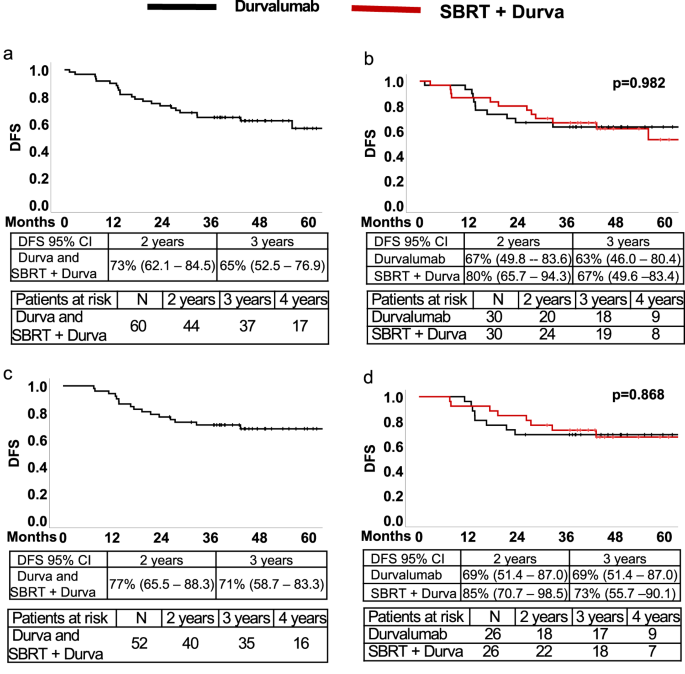
The authors previously reported the primary outcomes of a randomized phase II trial comparing neoadjuvant durvalumab (anti-PD-L1) alone or in combination with stereotactic radiotherapy in patients with early-stage NSCLC. Here, the authors report the secondary outcomes of the trial and post hoc...

