I guess you could say, "I told you so."
This cohort study identifies 5-year trajectories of opioid use for acute pain and cancer pain among US adults.

jamanetwork.com
"Overall, these findings suggest that most people who initiate an opioid prescription are likely to have low, time-limited exposure to opioids with little indication of ongoing use. This possibility is an important consideration for policymakers and stakeholders considering population-level prescribing of high-risk drugs. Opioids are essential drugs for acute and cancer pain, and many people with CNCP benefit from opioids.31 Continued focus and policy responses based on findings from a small group of people with increased risk of harms run the risk of limiting access to people who safely derive objective benefits from opioids."
Original Investigation Pharmacy and Clinical Pharmacology
August 10, 2023
Five-Year Trajectories of Prescription Opioid Use
Natasa Gisev, PhD1; Luke Buizen, MBiostat1; Ria E. Hopkins, MPH1; et alAndrea L. Schaffer, PhD2,3; Benjamin Daniels, PhD4; Chrianna Bharat, PhD1; Timothy Dobbins, PhD4; Sarah Larney, PhD5; Fiona Blyth, PhD6; David C. Currow, PhD7; Andrew Wilson, PhD8; Sallie-Anne Pearson, PhD4,8; Louisa Degenhardt, PhD1
Author Affiliations Article Information
JAMA Netw Open. 2023;6(8):e2328159. doi:10.1001/jamanetworkopen.2023.28159
Key Points
Question What are the 5-year trajectories of opioid use following initiation, and what are the characteristics of different trajectory groups?
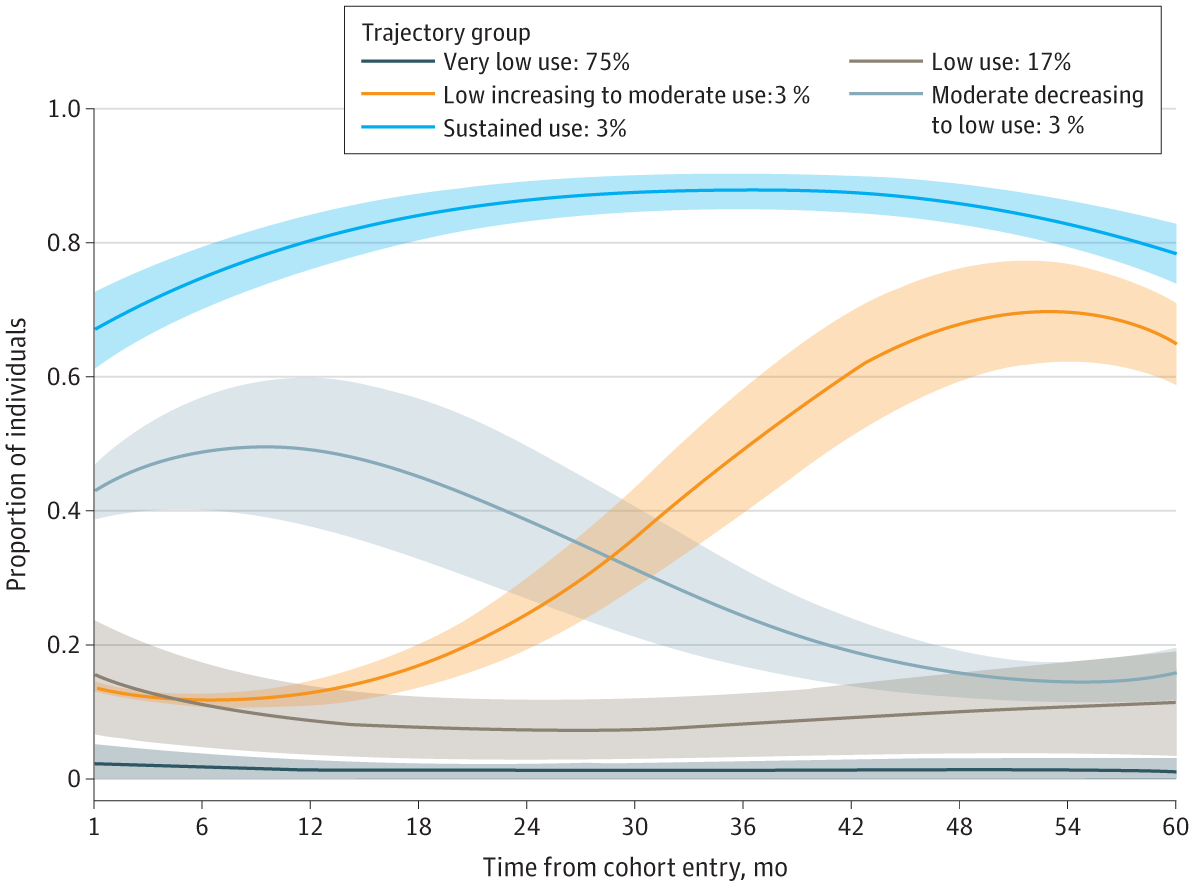
Findings In this population-based cohort study of 3.47 million adults, 5 trajectories of opioid use were identified. Approximately 3% of individuals were classified to the sustained use trajectory group, which was characterized by individuals with older age, a higher number of comorbidities, and higher use of psychotropic and other analgesic drugs and health services vs other trajectory groups.
Meaning Findings from this study suggest that, although most individuals who commenced prescription opioid treatment had low, time-limited exposure to opioids, the small proportion of adults with sustained or increasing opioid use had greater clinical complexity and treatment needs.
Abstract
Importance There are known risks of using opioids for extended periods. However, less is known about the long-term trajectories of opioid use following initiation.
Objective To identify 5-year trajectories of prescription opioid use, and to examine the characteristics of each trajectory group.
Design, Setting, and Participants This population-based cohort study conducted in New South Wales, Australia, linked national pharmaceutical claims data to 10 national and state data sets to determine sociodemographic characteristics, clinical characteristics, drug use, and health services use. The cohort included adult residents (aged ≥18 years) of New South Wales who initiated a prescription opioid between July 1, 2003, and December 31, 2018. Statistical analyses were conducted from February to September 2022.
Exposure Dispensing of a prescription opioid, with no evidence of opioid dispensing in the preceding 365 days, identified from pharmaceutical claims data.
Main Outcomes and Measures The main outcome was the trajectories of monthly opioid use over 60 months from opioid initiation. Group-based trajectory modeling was used to classify these trajectories. Linked health care data sets were used to examine characteristics of individuals in different trajectory groups.
Results Among 3 474 490 individuals who initiated a prescription opioid (1 831 230 females [52.7%]; mean [SD] age, 49.7 [19.3] years), 5 trajectories of long-term opioid use were identified: very low use (75.4%), low use (16.6%), moderate decreasing to low use (2.6%), low increasing to moderate use (2.6%), and sustained use (2.8%). Compared with individuals in the very low use trajectory group, those in the sustained use trajectory group were older (age ≥65 years: 22.0% vs 58.4%); had more comorbidities, including cancer (4.1% vs 22.2%); had increased health services contact, including hospital admissions (36.9% vs 51.6%); had higher use of psychotropic (16.4% vs 42.4%) and other analgesic drugs (22.9% vs 47.3%) prior to opioid initiation, and were initiated on stronger opioids (20.0% vs 50.2%).
Conclusions and relevance Results of this cohort study suggest that most individuals commencing treatment with prescription opioids had relatively low and time-limited exposure to opioids over a 5-year period. The small proportion of individuals with sustained or increasing use was older with more comorbidities and use of psychotropic and other analgesic drugs, likely reflecting a higher prevalence of pain and treatment needs in these individuals.