- Joined
- Nov 18, 2011
- Messages
- 330
- Reaction score
- 565
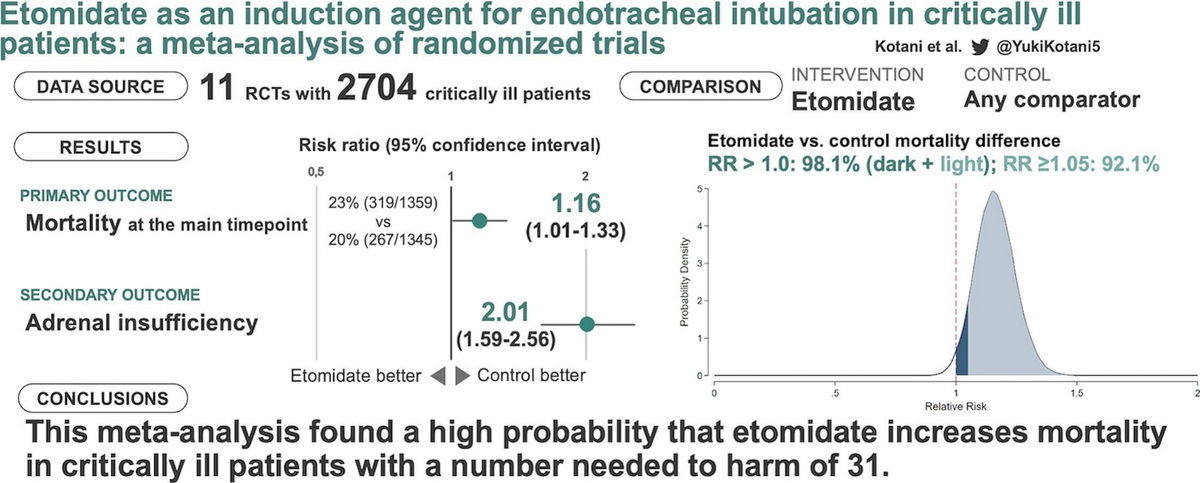
Etomidate as an induction agent for endotracheal intubation in critically ill patients: A meta-analysis of randomized trials
I was a big fan of Methohexital in the past, but my go-to lately has been etomidate now that I'm at a hospital where it's not available. Never been a huge fan of ketamine for induction, same with propofol though I've certainly used both. For any delayed sequence I'm not using etomidate anyway. This is a bummer, etomidate (aside from Brevital) was my favorite induction agent.
(PIC FROM META-ANALYSIS ABOVE)
I was a big fan of Methohexital in the past, but my go-to lately has been etomidate now that I'm at a hospital where it's not available. Never been a huge fan of ketamine for induction, same with propofol though I've certainly used both. For any delayed sequence I'm not using etomidate anyway. This is a bummer, etomidate (aside from Brevital) was my favorite induction agent.
(PIC FROM META-ANALYSIS ABOVE)

