- Joined
- Aug 18, 2017
- Messages
- 242
- Reaction score
- 290
PGY2 here. My experience has basically mostly been with depression addiction until now. I've been rotated to an acute ward and have more exposure now to psychosis (and obviously antipsychotics).
I'm having issues understanding the correct use of antipsychotics. Every attending has their own take on the subject and all of the sources I read postulate their own opinions and algorithms. Here is one of my current patients, with whom I'm having problems understanding how to proceed. As, I have the feeling, that we are managing him incorrectly.
Young patient with a known Schizoaffective disorder. He has been admitted multiple times, and had treated with Aripiprazol and lithium during his last stay (there's a long list of what he has had in the past). Due to extremely bad compliance, he decided to stop taking them abruptly.
He was readmitted because he developed imperative acoustic hallucinations. He was then started on Cariprazine 3mg/d because according to him, it was what helped him out the most in the past, and it's the only medication the patient would agree to take. He also had Diazepam and Haloperidol PRN. They were constantly used, but the patient refused to take anything else regularly.
After a few days, the hallucinations got better, but the patient became increasingly aggressive and delusional. Threatening other patients and even physically assaulting one. He has a past history of physical violence. A judge approved that we may withhold him for 4 weeks, and we can isolate him and restrain him when needed for the next week. But up until now he continues doing it in a "voluntary" basis.
He agreed with us on the need to escalate the medication and takes the medication voluntarily. Currently there is no legal basis to apply for involuntary medication.
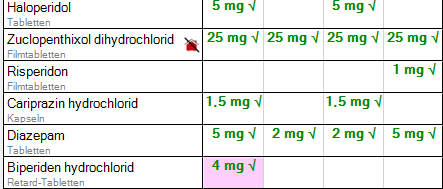
This is a picture of where we are currently at with the medication. Diazepam and Haloperidol were switch from PRN to regular medication. Our attending added Zuclopenthixol and According to him, the plan is to switch from Cariprazine to Risperidone. And eventually reduce Haloperidol, Zuclopenthixol and Diazepam.
And here I am, with little to no experience with antipsychotics and polypharmacy. But the little that I know is telling me that 4 antipsychotics are a red flag. I just wanted some input and advice. Thanks!
I'm having issues understanding the correct use of antipsychotics. Every attending has their own take on the subject and all of the sources I read postulate their own opinions and algorithms. Here is one of my current patients, with whom I'm having problems understanding how to proceed. As, I have the feeling, that we are managing him incorrectly.
Young patient with a known Schizoaffective disorder. He has been admitted multiple times, and had treated with Aripiprazol and lithium during his last stay (there's a long list of what he has had in the past). Due to extremely bad compliance, he decided to stop taking them abruptly.
He was readmitted because he developed imperative acoustic hallucinations. He was then started on Cariprazine 3mg/d because according to him, it was what helped him out the most in the past, and it's the only medication the patient would agree to take. He also had Diazepam and Haloperidol PRN. They were constantly used, but the patient refused to take anything else regularly.
After a few days, the hallucinations got better, but the patient became increasingly aggressive and delusional. Threatening other patients and even physically assaulting one. He has a past history of physical violence. A judge approved that we may withhold him for 4 weeks, and we can isolate him and restrain him when needed for the next week. But up until now he continues doing it in a "voluntary" basis.
He agreed with us on the need to escalate the medication and takes the medication voluntarily. Currently there is no legal basis to apply for involuntary medication.
This is a picture of where we are currently at with the medication. Diazepam and Haloperidol were switch from PRN to regular medication. Our attending added Zuclopenthixol and According to him, the plan is to switch from Cariprazine to Risperidone. And eventually reduce Haloperidol, Zuclopenthixol and Diazepam.
And here I am, with little to no experience with antipsychotics and polypharmacy. But the little that I know is telling me that 4 antipsychotics are a red flag. I just wanted some input and advice. Thanks!
